Abstract
Objective
The objective of this study was to evaluate the dosimetric impact on hypofractionated prostate radiation therapy of two geometric uncertainty sources: rectum and bladder filling and intrafractional prostate motion.
Materials and methods
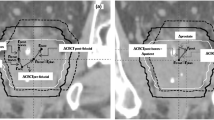
This prospective study included 544 images (375 pre-treatment cone-beam CT [CBCT] and 169 post-treatment CBCT) from 15 prostate adenocarcinoma patients. We recalculated the dose on each pre-treatment CBCT once the positioning errors were corrected. We also recalculated two dose distributions on each post-treatment CBCT, either using or not intrafractional motion correction. A correlation analysis was performed between CBCT-based dose and rectum and bladder filling as well as intrafraction prostate displacements.
Results
No significant differences were found between administered and planned rectal doses. However, we observed an increase in bladder dose due to a lower bladder filling in 66% of treatment fractions. These differences were reduced at the end of the fraction since the lower bladder volume was compensated by the filling during the treatment session. A statistically significant reduction in target volume coverage was observed in 27% of treatment sessions and was correlated with intrafractional prostate motion in sagittal plane > 4 mm.
Conclusions
A better control of bladder filling is recommended to minimize the number of fractions in which the bladder volume is lower than planned. Fiducial mark tracking with a displacement threshold of 5 mm in any direction is recommended to ensure that the prescribed dose criteria are met.






Similar content being viewed by others
References
Spratt DE, Pei X, Yamada J, Kollmeier MA, Cox B, Zelefsky MJ. Long-term survival and toxicity in patients treated with high-dose intensity modulated radiation therapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2013;85(3):686–92.
Palma D, Vollans E, James K, Nakano S, Moiseenko V, Shaffer R, et al. Volumetric modulated arc therapy for delivery of prostate radiotherapy: comparison with intensity-modulated radiotherapy and three-dimensional conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2008;72:996–1001. https://doi.org/10.1016/j.ijrobp.2008.02.047.
Zelefsky MJ, Kollmeier M, Cox B, Fidaleo A, Sperling D, Pei X, et al. Improved clinical outcomes with high-dose image guided radiotherapy compared with non-IGRT for the treatment of clinically localized prostate cancer. Int J Radiat Oncol Biol Phys. 2012;84:125–9. https://doi.org/10.1016/j.ijrobp.2011.11.047.
Zapatero A, Roch M, Büchser D, Castro P, Fernández-Banda L, Pozo G, et al. Reduced late urinary toxicity with high-dose intensity-modulated radiotherapy using intra-prostate fiducial markers for localized prostate cancer. Clin Transl Oncol. 2017;19:1161–7. https://doi.org/10.1007/s12094-017-1655-9.
Ghilezan M, Yan D, Liang J, Jaffray D, Wong J, Martinez A. Online image-guided intensity-modulated radiotherapy for prostate cancer: How much improvement can we expect? A theoretical assessment of clinical benefits and potential dose escalation by improving precision and accuracy of radiation delivery. Int J Radiat Oncol Biol Phys. 2004;60:1602–10. https://doi.org/10.1016/j.ijrobp.2004.07.709.
Brenner DJ, Hall EJ. Fractionation and protraction for radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys. 1999;43:1095–101.
Fowler J, Chappell R, Ritter M. Is alpha/beta for prostate tumors really low? Int J Radiat Oncol Biol Phys. 2001;50:1021–31.
Williams SG, Taylor JMG, Liu NG, et al. Use of individual fraction size data from 3756 patients to directly determine the alpha/beta ratio of prostate cancer. Int J Radiat Oncol Biol Phys. 2007;64:24–33.
Proust-Lima C, Taylor JM, Sécher S, et al. Confirmation of a low alpha/beta ratio for prostate cancer treated by external beam radiation therapy alone using a post-treatment repeated-measures model for PSA dynamics. Int J Radiat Oncol Biol Phys. 2010;79:195–201.
Miralbell R, Roberts SA, Zubizarreta E, et al. Dose–fractionation radiosensitivity of prostate cancer deduced from radiotherapy outcome of 5969 patients in seven international institutional datasets. Int J Radiat Oncol Biol Phys. 2009;75:S81.
Vogelius IR, Bentzen SM. Meta-analysis of the alpha/beta ratio for prostate cancer in the presence of an overall time factor: bad news, good news, or no news? Int J Radiat Oncol Biol Phys. 2013;1:89–94.
Arcangeli S, Strigari L, Gomellini S, Saracino B, Petrongari MG, Pinnarò P, et al. Updated results and patterns of failure in a randomized hypofractionation trial for high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2012;84:1172–8.
Wilkins A, Mossop H, Syndikus I, Khoo V, Bloomfield D, Parker C et al. Hypofractionated radiotherapy versus conventionally fractionated radiotherapy for patients with intermediate-risk localised prostate cancer: 2-year patient-reported outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol. https://doi.org/10.1016/S1470-2045(15)00280-6
Thor M, Deasy JO, Paulus R, Robert Lee W, Amin MB, Bruner DW, et al. Tolerance doses for late adverse events after hypofractionated radiotherapy for prostate cancer on trial NRG Oncology/RTOG 0415. Radiother Oncol. 2019;135:19–24. https://doi.org/10.1016/j.radonc.2019.02.014.
Pollack A, Walker G, Horwitz EM, Price R, Feigenberg S, Konski AA, et al. Randomized trial of hypofractionated external-beam radiotherapy for prostate cancer. J Clin Oncol. 2013;31:3860–8.
Jereczek-Fossa BA, Surgo A, Maisonneuve P, Maucieri A, Gerardi MA, Zerini D, et al. Late toxicity of image-guided hypofractionated radiotherapy for prostate: non-randomized comparison with conventional fractionation. Radiol Med. 2019;124:65–78. https://doi.org/10.1007/s11547-018-0937-9.
Roch M, Zapatero A, Castro P, Büchser D, Pérez L, Hernández D, et al. Impact of rectum and bladder anatomy in intrafractional prostate motion during hypofractionated radiation therapy. Clin Transl Oncol. 2019;21:607–14.
Castro P, Roch M, Zapatero A, Büchser D, Garayoa J, Ansón C, et al. Multicomponent assessment of the geometrical uncertainty and consequent margins in prostate cancer radiotherapy treatment using fiducial markers. Int J Med Phys Clin Eng Radiat Oncol. 2018;07:503–21.
Chen Z, Yang Z, Wang J, Hu W. Dosimetric impact of different bladder and rectum filling during prostate cancer radiotherapy. Radiat Oncol. 2016;11:1–8. https://doi.org/10.1186/s13014-016-0681-z.
Pearson D, Gill SK, Campbell N, Reddy K. Dosimetric and volumetric changes in the rectum and bladder in patients receiving CBCT-guided prostate IMRT: analysis based on daily CBCT dose calculation. J Appl Clin Med Phys. 2016;17:107–17.
McParland N, Pearson M, Wong J, Sigur I, Stenger C, Tyldesley S. Quantifying daily variation in volume and dose to the prostate, rectum and bladder using cone-beam computerised tomography. J Radiother Pract. 2014;13:79–86.
Murthy V, Shukla P, Adurkar P, Master Z, Mahantshetty U, Shrivastava SK. Dose variation during hypofractionated image-guided radiotherapy for prostate cancer: planned versus delivered. J Cancer Res Ther. 2011;7:162–7.
Kupelian PA, Langen KM, Zeidan OA, Meeks SL, Willoughby TR, Wagner TH, et al. Daily variations in delivered doses in patients treated with radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2006;66:876–82.
Funding
This work has not specific funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All the authors have contributed sufficiently to the scientific work and therefore share collective responsibility and accountability for the results. All the authors have read, approved, and consented to submit the manuscript. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent is not required for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roch, M., Zapatero, A., Castro, P. et al. Dosimetric impact of rectum and bladder anatomy and intrafractional prostate motion on hypofractionated prostate radiation therapy. Clin Transl Oncol 23, 2293–2301 (2021). https://doi.org/10.1007/s12094-021-02628-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-021-02628-3